Infectious Spondylitis
Introduction
Although the human vertebrae is protected and shielded from the external world, in rare instances, it can be infected by bacteria or other microbes. This leads to infectious spondylitis. Despite its rarity, it could turn out to be dangerous and potentially lethal. Patients of this ailment will experience swelling and tenderness in the back, high fever, chills and night sweats.
This pathology can occur as a result of a recent surgery where proper sterilization measures were not taken. It can also happen because the immune system is compromised. In some cases, it can also be brought on by a dental procedure, intravenous drug use, or the use of a catheter. Furthermore, it can also be caused by an infection spreading from another part of the body to the spine. Irrespective of the cause, prompt treatment in the case of infectious spondylitis is absolutely necessary.
Symptoms
Infectious spondylitis encompasses a range of symptoms, often causing uneasiness and affecting daily life.
- Chronic back pain, often intense and localized.
- Swelling and numbness around the affected area.
- Stiffness in the morning or after prolonged periods of inactivity.
- Fever, chills, and extreme weight loss.
- Restricted mobility due to pain.
- Muscle stiffness around the spine.
- Neurological symptoms like numbness if spinal nerves are impinged.
Causes
Infectious spondylitis occurs when an infection spreads to the spine, leading to inflammation.
- Bacterial infections, most commonly Staphylococcus aureus.
- Tuberculosis infection, particularly in developing countries (Pott’s disease).
- Fungal infections, though rare, can also affect the spine.
- Spread of infection from other parts of the body, such as urinary tract or respiratory infections.
- Post-surgical infections or complications from spinal procedures.
- Intravenous drug use, can introduce bacteria into the bloodstream.
- Weakened immune system, increasing susceptibility to infections.
Diagnosis and Treatment
Early diagnosis and timely treatment are crucial to dealing with infectious spondylitis well.
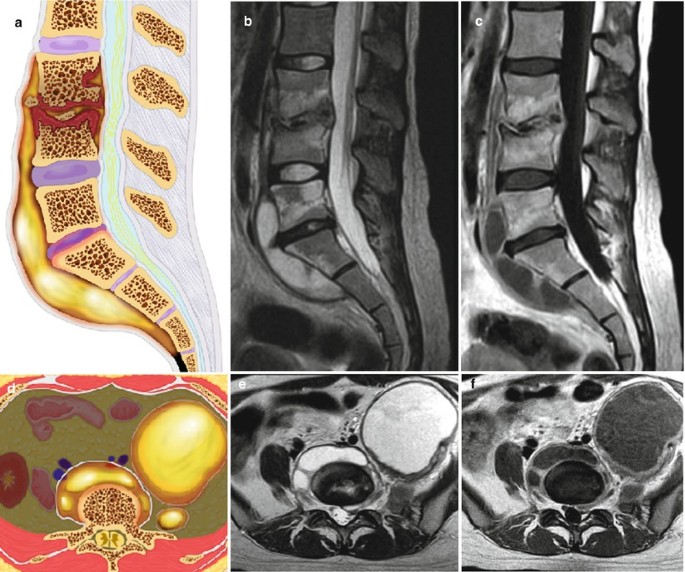
- A thorough diagnosis consists of imaging tests such as MRI or CT scans, blood tests to identify infection markers (elevated ESR, CRP), and a physical examination to evaluate pain and neurological function.
- To isolate the microbe causing the infection, a biopsy or culture test may be carried out.
- Management entails targeted antibiotic or antifungal therapy, and anti-inflammatory drug for pain alleviation.
- In extreme situations, surgery will be needed to empty abscesses or stabilize the spine. Rehabilitation exercises would then be required to strengthen the back and restore mobility.
Risk Factors
Several factors can increase the chance of developing infectious spondylitis. They are:
- Degenerative disc disease and other pre-existing spinal disorders.
- Old age, since aging weakens the immune system.
- Diabetes or long-term illnesses that weaken the immune system.
- History of invasive procedures or spinal surgery.
- Inadequate personal hygiene or risky behaviors among intravenous drug users.
- Malnourishment or long-term immunosuppressive drug use.
- Living in an area where tuberculosis is highly prevalent.
